COMPUTATIONAL PSYCHIATRY AND NEUROLOGY
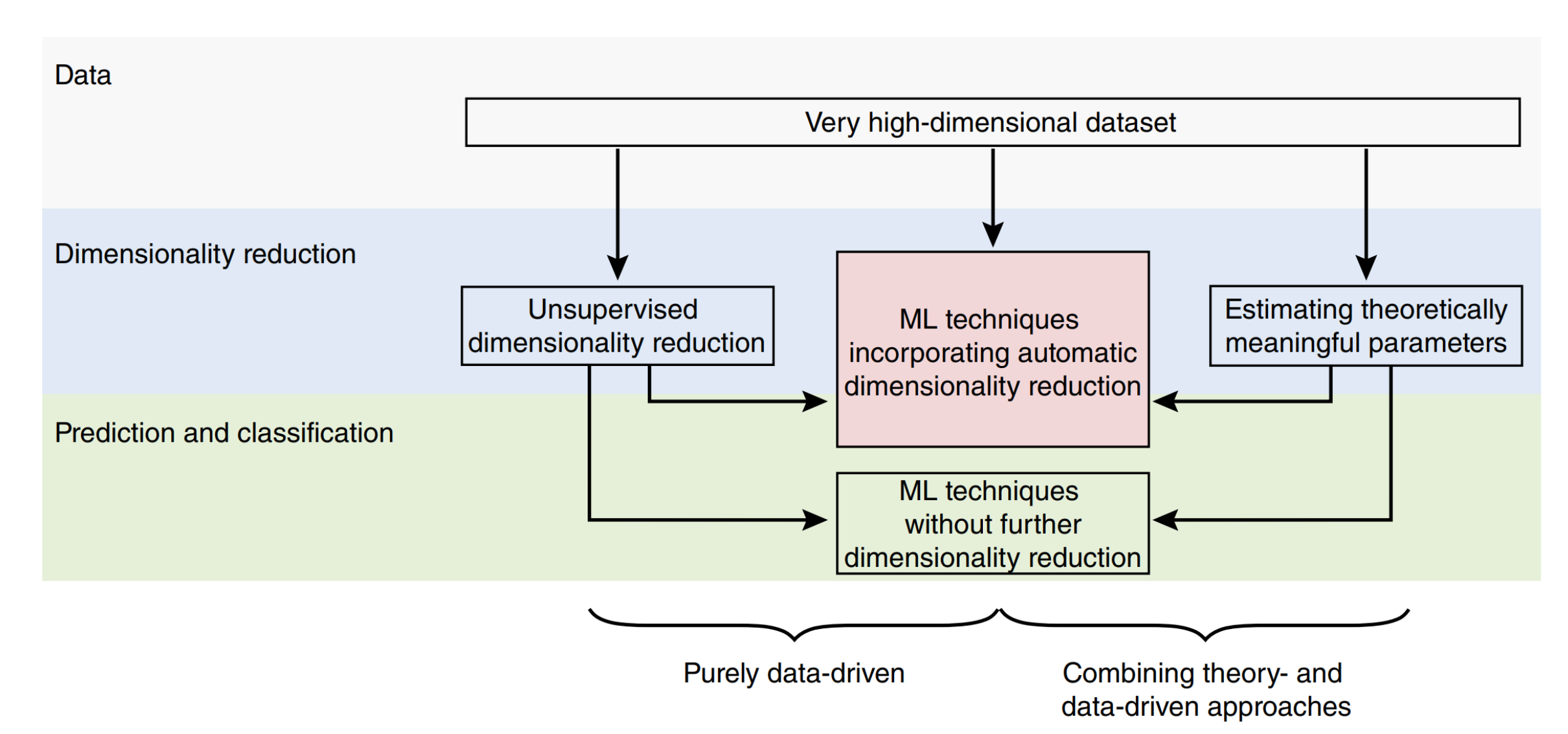
Given the importance of learning, decision making, and cognitive control in adaptive cognition and comportment, it has proven very valuable to apply our models towards understanding serious mental illnesses. We have contributed to the emerging field of computational psychiatry and neurology, which aims to further this endeavor by applying multiple levels of computation, theory, and machine learning to improve diagnostic classification and treatment. Our earlier work generated enthusiasm for this approach by identifying mechanisms within dynamical neural models, and algorithmic descriptions thereof, that can explain pathological behaviors across several disorders (Maia & Frank, 2011; Wiecki, Poland, & Frank, 2015; Huys, Maia, & Frank 2016). We have articulated four complementary strategies for deriving and testing hypotheses about mechanisms of these disturbances across levels of analysis. We also consider the utility of combining “machine learning” (modern statistical) approaches based on cognitive and neural markers with theory-driven models for classification of individual patients. We situate this problem in the context of the current psychiatric classification system, and then describe data-driven methods that can cluster and classify subjects based on quantitative model parameters fit to behavioral and neural data. We present a proof-of-concept that these methods can improve identification of relevant clinical variables, and that they are superior to classification based on the raw data alone. We have drawn similar conclusions in other quantitative investigations in both simulation and real data in pre-symptomatic Huntington’s disease, Parkinson’s disease, and healthy aging (Wiecki et al., 2015; 2016). This approach therefore shows promise toward development of more effective, principled diagnostic and therapeutic strategies, while also providing a metric for the utility of a model more generally (i.e., the degree to which it can improve classification).
Schizophrenia
Application of computational psychiatry approaches to schizophrenia, a complex heterogeneous illness, has led to a re-valuation of the intersection between negative symptoms (e.g. anhedonia) and cognitive deficits as well as the impact of anti-psychotic drugs on those processes. We have also used refined paradigms and computational models to disentangle different mechanisms contributing to otherwise seemingly unitary behavioral processes. This work proffers the exciting possibility of a mechanistic understanding of an unmet clinical need – the apathy associated with chronic mental illnesses.